Researchers at Imagine Pharma, a regenerative medicine company based in Pittsburgh, Philadelphia, have engineered pancreatic cells from someone with long term type 1 diabetes and enabled them to produce insulin.
While the work is still in its early stages, if validated it could allow a patient’s own cells to be used to treat type 1 diabetes and create functioning pancreatic cell transplants without risk of rejection.
Academic and industry researchers and clinicians have investigated the possibility of transplanting functional insulin producing beta cells into the pancreas of patients with type 1 diabetes, who gradually lose the function of these cells after diagnosis, for many years. However, many such attempts have failed due to rejection issues and problems with collecting enough viable cells for transplantation.
Autologous cell therapy, where a patient’s cells are extracted, re-engineered and returned to the body to treat a condition or disease, has developed enormously in recent years, particularly in the field of cancer with cell therapies such as chimeric antigen receptor (CAR)-T cells reaching the market.
Imagine Pharma is attempting to do something similar with type 1 diabetes. Researchers at the company reported this week at the American Transplant Congress in Boston that they have succeeded in creating type 1 diabetes Activated Islet Progenitor Cells (T1D-AIPCs) in the lab that are capable of producing both insulin and glucagon.
“We envision that our novel cell population of T1D AIPCs holds tremendous potential for the treatment and cure of type 1 diabetes via autologous cell transplantation,” said Ngoc Thai, Imagine Pharma’s Founder, co-CEO, and CMO.
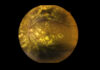
The T1D-AIPCs cells were generated from pancreatic biopsies taken from a 58-year-old deceased organ donor who was diagnosed as a child and had diabetes for 53 years.
After generating the T1D-AIPCs in the lab, the team used mRNA analysis to check for insulin and glucagon production. When the cells were shown to be viable and insulin producing, the team implanted them into a mouse model of type 1 diabetes (NOD-Scid) to assess if they could restore insulin production, which was successful.
Notably, Imagine Pharma has also discovered a method to produce these cells in big enough quantities to make a viable cell therapy, a problem that has blocked similar attempts in the past.
The researchers also found quantities of biomarkers in the cells grown in the lab that suggest that they could go on to form functional pancreatic islet cells including a range of pancreatic transcription factors, the islet neogenesis factor nestin, the glucose transporter Glut-2, the secretory product of beta-cells IAPP, and somatostatin.
“This study provides the ground work and approach for the generation and treatment of type 1 diabetes in the setting of an autologous cell transplantation,” conclude the investigators.